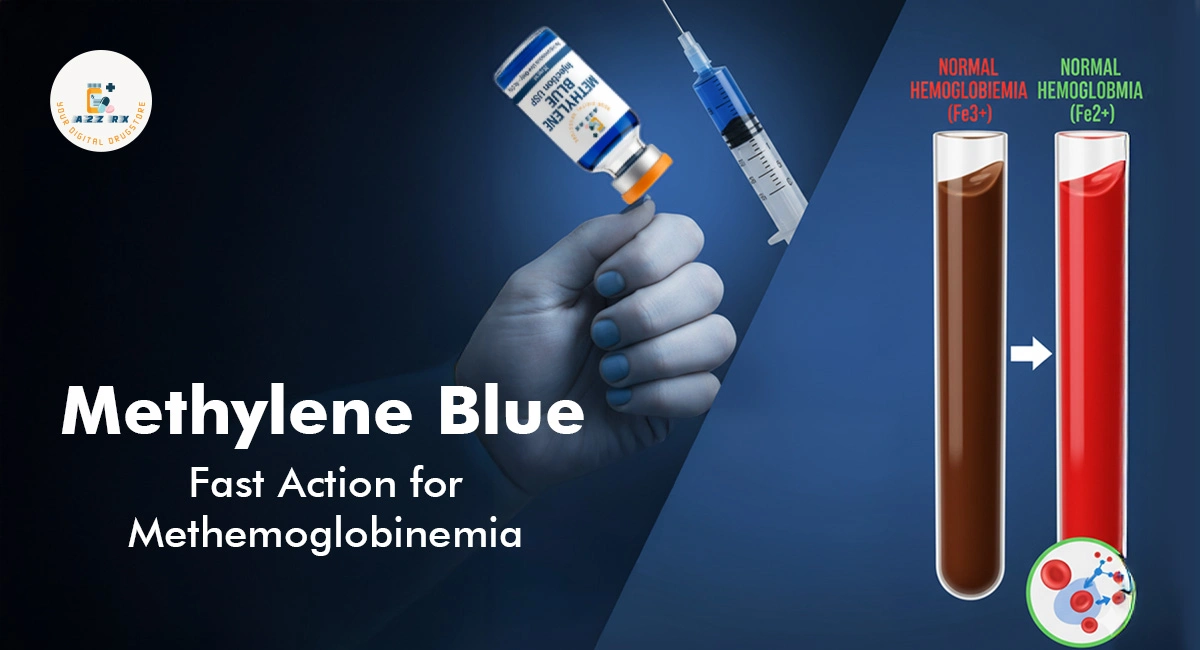
Methemoglobinemia is a serious—but
treatable—blood disorder in which the iron in hemoglobin is oxidized from the
ferrous (Fe²⁺) form to the ferric (Fe³⁺) form. That ferric form (methemoglobin)
can’t bind oxygen effectively, reducing oxygen delivery to tissues. In many
cases, methylene blue injection USP is the first‑line antidote. Below,
we explore how it works, dosage guidelines, benefits, risks, and how patients
might locate it (for example, via A2Z RX).
How Methylene Blue Works: Mechanism of
Action
When given intravenously, methylene blue is
reduced to leucomethylene blue, which then acts as an electron donor to
convert methemoglobin (Fe³⁺) back to functional hemoglobin (Fe²⁺). Accelerates
oxygen delivery to tissues, restoring normal oxygenation.
In effect, methylene blue supplements the
body’s own reductase systems (e.g., NADPH‑dependent methemoglobin reductase).
It is beneficial when those systems are overwhelmed by exposures to oxidizing
agents (e.g., certain drugs, nitrates).
Indications & When It Is Used
Methylene blue injection USP is indicated when:
- Methemoglobin levels are significantly elevated (often
> 30 %), or
- Patients show clinical signs of hypoxia (cyanosis, shortness of
breath, fatigue) that do not improve with oxygen.
It is essential when methemoglobinemia is
acquired (from drug exposures) or when the patient fails to improve via
supportive measures.
Dosage Guidelines & Strengths
The commonly recommended dose is 1 mg/kg
IV of a 1% methylene blue solution, administered slowly over 5 to 30
minutes. If methemoglobin levels remain high or symptoms persist after one
hour, a second dose may be considered.
Some sources allow a broader range
(1-2 mg/kg) depending on severity.
Methylene blue is often supplied in vials
at 50 mg per 10 mL (i.e., 5 mg/mL).
In many clinical protocols, only one or two
doses are used—higher or repeated dosing carries risk.
Benefits & Clinical Importance
- Rapid reversal of methemoglobinemia: Methylene blue can reduce methemoglobin levels within minutes,
restoring oxygenation.
- Life‑saving in severe cases: For
patients with severe hypoxia or symptomatic methemoglobinemia, MB is often
the most effective immediate therapy.
- Well-understood antidote: Its
mechanism and efficacy in this indication are well documented in medical
literature.
Because of its potency, speed, and
relatively well-characterized safety profile (when used at appropriate doses),
methylene blue remains the standard therapy for many cases of
methemoglobinemia.
Risks, Contraindications & Safety
Considerations
Even though it is a powerful antidote,
methylene blue is not free of risks. Key safety points include:
- G6PD deficiency is a contraindication. In patients with glucose-6-phosphate dehydrogenase deficiency,
methylene blue may provoke hemolytic anemia and worsen the patient’s
condition.
- Hypersensitivity or allergy to
methylene blue or related dyes prohibits its use.
- Serotonin syndrome risk: Methylene
blue is a weak monoamine oxidase inhibitor (MAOI). When used concomitantly
with serotonergic medications (e.g., SSRIs, SNRIs, certain
antidepressants), there is a recognized risk of serotonin syndrome.
- Interference with monitoring: After
methylene blue administration, pulse oximetry readings may become
inaccurate (due to dye interference). Arterial blood sampling may be
required for accurate oxygenation assessment.
- Hematologic risk: In rare cases,
hemolysis or methemoglobinemia rebound may occur with excessive doses.
- Dose-related toxicity: At high
doses, methylene blue may act as an oxidant, paradoxically contributing to
methemoglobin formation or other toxic effects.
Because of these risks, careful
calculation, medical monitoring, and use of the minimal effective dose are
critical.
How to Obtain & Pricing: “Methylene
Blue Injection Near Me” & Market Notes
If someone is searching for MethyleneBlue Injection near me, or wants to know the Methylene Blue Injection
price, here are some practical points:
- Pharmacy/hospital supply: Methylene
blue is typically stocked in hospital pharmacies and specialty compounding
pharmacies rather than general retail drugstores.
- Compounded or USP grade: One must
ensure the product is USP grade (pharmaceutical standard) for
injection. Substandard or non‑USP forms may contain impurities.
- Transparent pricing: Institutions
or specialty pharmacies may list the price of the methylene blue
injection or provide quotes based on strength (e.g., 25 mg or 50 mg
vials).
- Tailored procurement via A2Z RX: If
A2Z RX offers sourcing or compounding services, patients or providers may
consult to obtain a legitimate USP Methylene Blue Injection under
prescription and regulatory compliance.
A typical vial strength used clinically is 25 mg
or 50 mg (depending on the manufacturer), though local availability may
vary.
Summary & Final Notes
Methylene blue injection USP plays a pivotal role in treating methemoglobinemia,
converting dysfunctional methemoglobin back to active hemoglobin and restoring
tissue oxygenation. The standard dose is about 1 mg/kg IV, with
carefully limited repeat dosing if needed. However, use must be cautious due to
contraindications (especially in G6PD deficiency), risk of hemolysis,
interaction with serotonergic agents, and interference with monitoring devices.
If you or your medical practice is
considering obtaining methylene blue injection USP, working with
authorized providers, ensuring pharmaceutical quality, and verifying methylene
blue dosage and safety protocols is essential. Clinics or pharmacies
seeking to stock it should ensure correct handling, storage, and administration
practices.